Despite the dramatic improvement in haemophilia treatment over the last decades, there are still several unmet needs in the management of patients with haemophilia: The requirement of regular intravenous infusion of the missing factor, the development of inhibitors and the development and progression of haemophilic arthropathy despite regular prophylaxis. Furthermore, even though it is a monogenic disease, haemophilia is characterised by a wide spectrum of bleeding severity which cannot be explained by the deficient or missing coagulation factor alone. Therefore, a personalised approach to patients is mandatory to address individual patient needs.
The objective of the project PERSEPHONE has been to implement a personalised approach for the optimal multidisciplinary care of haemophilic patients. With the collaboration of the company Your Business Partner (YBP) we re-designed the management pathway based on a Value Based Healthcare (VBH) approach. Conversations were conducted with different patients following an anthropological approach to maximize both the clinical outcome and the patient experience (Figure 1).
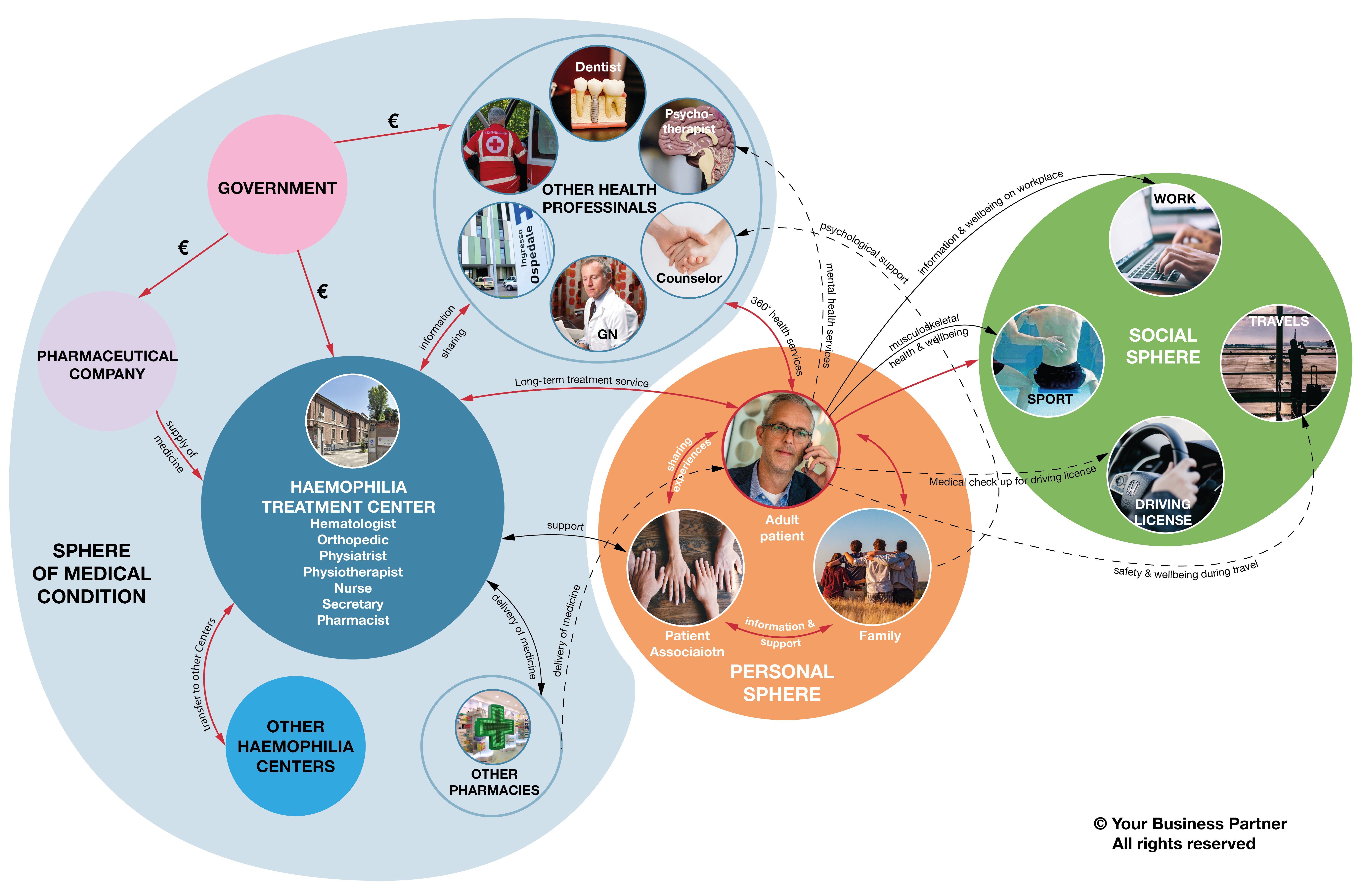
The multidisciplinary team is composed of a haematologist, a rheumatologist, an orthopaedic and a physiotherapist. With this programme, each patient is followed since the diagnosis, during the growth process, with continuous adjustment of treatment based on the individual characteristics and the personal needs of each patient. The 24h-availability of haematologists for emergency allows the immediate management of acute bleeding and musculoskeletal injuries. Every week, the multidisciplinary team meets for the check-up of patients affected by haemophilia.
Both clinical and laboratory parameters are taken into account. A pharmacokinetics curve of the factor replacement drug is performed in order to check the appropriateness of the treatment. The genomic profile of haemophilic patients is useful not only for the diagnosis, but also for the prediction of inhibitor development, to assess the risk for bleeding complications and therefore to select the best product for each patient.
The musculoskeletal program aims to monitor the joint health of patients, to improve their quality of life, and to increase the functional independence of patients from childhood to the adult age. An accurate physical and ultrasound evaluation of the main joints involved in haemophilic arthropathy is performed. From the orthopaedic surgical point of view, through innovative Computer Tomography studies and the use of 3D printers, custom-made prosthetic models that accurately reproduce the patient's anatomy have been developed and implemented, taking into account the individual characteristics of the joint of each patient.
The physiotherapist examination consists of a postural analysis, baropodometric and stabilometric platform analysis, quality of life assessment and a survey of the daily physical and recreational activities. Based on all these objective clinical data, on the individual patient’s needs, preference and motivational aspect, the patient is advised to follow a targeted physiotherapy program or sport activity. During the first wave of the COVID-19 pandemic, video call system for remote examination of the patient and a telehealth program of rehabilitation have been implemented to maintain physical activities in these patients.
We are currently designing an electronic medical record that will collect genetic, phenotypic, medical history, physical activity, joint health by ultrasound and pharmacokinetics and treatment data. The use of a predictive algorithm based on these data will allow us to define the best treatment for each individual. Furthermore, a telehealth approach will be implemented that uses home-based musculoskeletal ultrasound and machine learning programmes based on imaging for early detection of joint bleeding. This will allow to personalise treatment and on the one hand avoid overtreatment in the absence of joint bleeding, while on the other hand avoiding undertreatment due to underestimated joint bleeding.
“The PERSEPHONE project envisages a novel model of multidisciplinary hemophilia care based on the personalised management of the patient that takes into account genetic data, individual pharmacokinetics profile, lifestyle and joint health by ultrasound imaging. The COVID-19 pandemic has taught us the importance of a telehealth approach. We hope we will soon provide the patients with telemedicine instruments such as home-based joint ultrasound monitoring and serum biomarkers that will integrate hospital-based management with the ultimate goal to improve the personalised treatment of these patients.”
Prof. Flora Peyvandi
The exchange with other specialists, with academia and with drug producers involved in this project is constant and continuous, aimed at the improvement of the quality of care of patients. The model of the Centre could be replicable in other locations. A necessary condition is the collegial management of the patient, the dialogue among the members of the team, the education of the specialists involved and the presence of suitable spaces for the logistic organization of the Center.

